Resource • Article
Site Selection: Building a Bridge with Clinical Sites During COVID-19 Studies


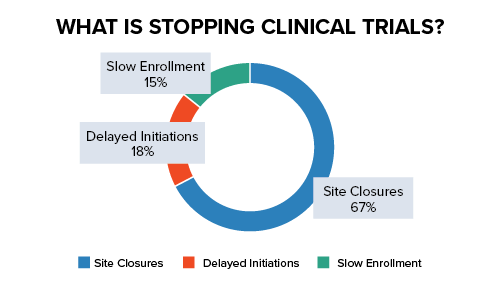
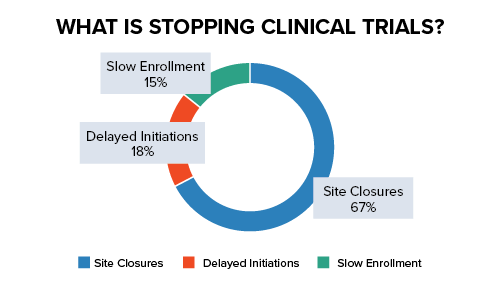
Clinical sites are the backbone of clinical trial execution. As the physical presence of study operations, sites manifest the purpose of pharmaceutical companies, CROs, and patients alike. However, the rise of COVID-19 has severely impacted the ability of clinical sites to perform their most basic research functions, causing major delays, forcing closures, and limiting capabilities. See Figure 1 below.
Figure 1
The search for coronavirus vaccines in the midst of the pandemic has created the need for a bridge – to connect drug developers and patient subjects and facilitate viable research. Clinical sites are that bridge; however, managing expectations and availability should be part of early due diligence for vaccine and treatment developers and addressed well ahead of trial execution.
Site Identification and Availability
The first step in working with clinical sites for COVID-19 trials involves site identification and selection. No site feasibility effort would be complete without an understanding of the disease, and specifically how that disease presents itself epidemiologically. This information allows drug and device developers to target sites in areas where the disease is most prevalent. The current map of pandemic cases (see Figure 2 below) highlights the global hot zones for COVID-19.
Figure 2
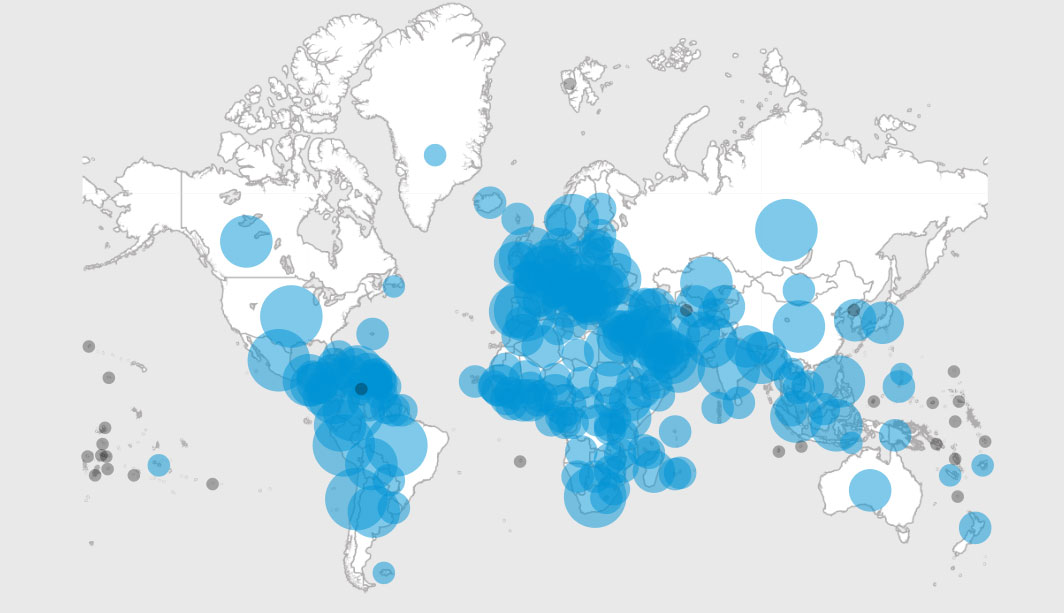
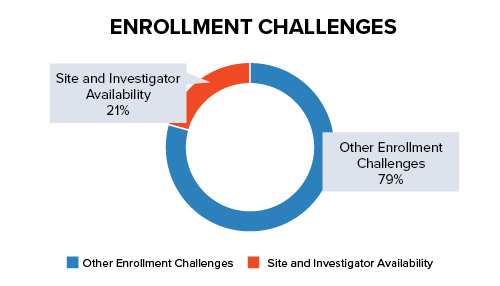
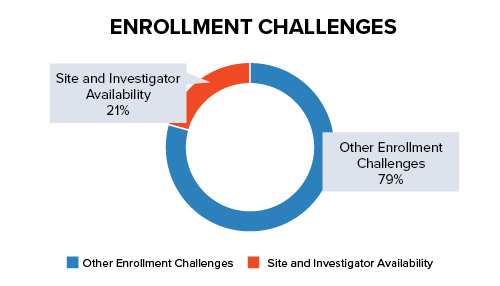
However, epidemiological data can be misleading. While a location with a large number of patients may seem like a prime target for recruiting and conducting COVID-19 studies, large hot zone patient pools may present challenges:
- During a pandemic, resources including site staff and equipment can often be redirected to focus on the public health aspect of the emergency and away from clinical research.
- Additionally, sites that are available for research are in greater demand, leading to limited availability and responsiveness.
- Hot zone locations can provide access to a large population of potential participants. However, sites and resources can be impacted by local safety regulations and governance.
COVID-19 is also an especially difficult disease to track because, as it is a particularly infectious disease, the hot zones where case counts are increasing are ever-shifting. Accommodating the nuance of coronavirus trials in this situation requires speed and agility. Prior to committing to trial execution, site identification and selection must become the priority. Strategies should focus on contingencies:
- Investigating a large number of potential sites on a global scale to determine which sites are open or not previously engaged
- Maintaining open lines of communication with current site partners to understand their upcoming trial schedule and capacity
- Confirming that sites can accommodate COVID-19 safety protocols for vaccine and treatment studies
- Establishing a communication line with sites in the early stages of assessment, allowing frequent updates on the information that will ultimately drive successful recruitment outcomes: number of new cases per week, number of competing studies accepted, etc.
COVID-19 Regulatory Guidance for Clinical Sites
When considering a group of clinical sites for COVID-19 trials, consider each location’s strategy for mitigating risk during the study. While good clinical practice (GCP) and operational efficiency are universal standards for safety and data integrity, the FDA and other international regulatory agencies now task clinical sites with further guidelines to remain compliant.
Chief among these are safety measures for patients and clinical site staff. GCP protocols for all types of clinical trials are focused on the health and welfare of patients. Coupled with the risk of COVID-19 infection for site investigators, monitors, and staff, vaccine trials may require further guidelines:
- For Patients – Per the FDA, “ensuring the safety of trial participants is paramount.” And while infected patients with severe symptoms may be confined to a hospital or clinical site, asymptomatic patients and those with mild symptoms may be quarantined at home. Sites, and their sponsors, have the responsibility of maintaining safety during the trial. This can include:
- Assessing the site location infection rate to determine if the area is in a COVID-19 hot zone
- Communicating trial protocol changes caused by COVID-19 with study participants prior to trial execution
- Determining if decentralization strategies – such as virtual trials and other alternative solutions – would be an applicable and/or practical solution for maintaining patient safety and trial milestones
- For Site Staff – Conducting COVID-19 and other types of clinical trials are a team effort. Site staff are a valuable component and must be protected accordingly. Apart from mandatory training in COVID-19 prevention, staff should also acknowledge the following:
- Understanding site protocol and potential risks to patients and other staff members
- Facilitating changes to the site’s physical structure, ensuring testing and other areas accommodate physical distancing when applicable
- Screening patients for coronavirus prior to site visits and at agreed upon intervals during clinical trials
- Ascertaining which parts of the trial can be decentralized, including the use of telemedicine and eSourcing technology
- Providing contingency access to CRAs and auditors – through remote monitoring solutions – for scheduled visits
Additionally, strategies for outsourcing to labs, for the processing of bloodwork and study specimens, must be reviewed prior to trial execution. Clinical research labs must follow similar guidance for occupational exposure as clinical sites, including OSHA and CDC biosafety guidelines.
Assessing Decentralization Options
Sites and their sponsors may find it necessary to consider decentralization strategies during a COVID-19 trial. It is important to note that decentralization options consist of a spectrum of solutions, ranging from remote monitoring to full virtual trials. The degree to which remote, virtual, and decentralized solutions can be implemented depends heavily on the patient population, the site’s own safety protocols, and of course the study protocol. For example, telemedicine components may be required when planning a trial in a symptom management protocol for a patient population with mild disease, but not applicable when planning a study in a patient population who is hospitalized.
Consider another example – a clinical site selected for a COVID-19 vaccine trial has been compromised by infection within the site and the surrounding locale. The following questions would need to be answered in order to avoid delays to the study timeline:
- Does the site have an infection control or contingency plan? If the site goes into lockdown until the infection is eliminated, it is important to the viability of the vaccine study to know the length of the downtime. Additionally, communication with the site would determine the need for the transfer of operations to an adjacent, active site on a temporary/permanent basis.
- Are there alternatives to physical site visits for patients? To ensure continuity and safety measures, sites must be prepared to support decentralized solutions for patients if necessary, including telemedicine, home care visits, eSourcing, and other options. This includes site staff support as well as technology needs.
- Is on-site monitoring available and appropriate? Data integrity and validity should be a key concern for sites, and risk mitigation strategies should be actionable. This must include alternatives such as remote monitoring for CRAs, digital transmission of clinical documentation, and remote data capture.
Building a Better Bridge
Clinical sites represent the connection forged between all trial stakeholders during clinical trials, and this is especially true for coronavirus studies. Sponsors are learning that all elements of COVID-19 are in a state of constant flux, and that having a reliable pool of sites to engage with is a necessity to complete each determined step in vaccine testing. Through proper due diligence, sponsors will find clinical sites that are held in high regard for their safety and compliance measures, their understanding of disease epidemiology, and their ability to adapt to novel experiences – a smart strategy for ensuring a solid and flexible bridge for executing COVID-19 trials.
Recognizing clinical site value is only one part of the execution strategy for COVID-19 trials. Our next article will focus on regulatory timelines and fast-tracking coronavirus vaccines. Click here to learn more in the Biorasi COVID-19 Article Series.
References
- Adams, Ben. “More than two-thirds of trials hit by COVID-19 enrollment halts, with midstage tests the worst affected.” Fierce Biotech, July 1, 2020.
- World Health Organization. “WHO Coronavirus Disease (COVID-19) Dashboard.” Updated August 10, 2020.
- Joseph, Andrew. “Efforts to beat back the coronavirus are critical. They’re also making clinical trials harder.” Stat News, May 5, 2020.
- S. Food & Drug Administration. “FDA Guidance on Conduct of Clinical Trials of Medical Products during COVID-19 Public Health Emergency.” July 2, 2020.
- Novara, Daniele. “Coronavirus pandemic (COVID-19) – Clinical trials advice.” Open Access Text, April 8, 2020.